What the mips is going on here…
MIPS…it’s not the latest slang for a curse word (although maybe it should be). Get the mips out of here. Mind your own mipsing business. I’ll be right back, I need to take a mips. No…MIPS is the newest Medicare quality reporting program – thank you President Obama.
What is MIPS
Merit-based Incentive Payment System (MIPS) replaces the previous quality reporting programs that we have become so fond of – Physician Quality Reporting Program (PQRS), Value-Based Payment Modifier (VM) and Medicare Electronic Health Records (EHR) Incentive Program. If you see any Medicare Part B patients it is important to understand what MIPS is and how it will affect you.
In 2015, the Medicare Access and CHIP Reauthorization Act (MACRA) was signed into place with the hopes of controlling the cost of Medicare payments. Prior to the advent of MACRA clinicians were paid based on a fee-for-service payment system – you got paid for what you did. The more you saw (larger volume) the more you were paid. Instead of a fee-for-service payment system MACRA aims to incentivize value over volume.
Most physicians, PAs, NPs, clinical nurse specialist and certified registered nurse anesthetists will be required to participate in MIPS for years 1 and 2 of the program; beyond that other eligible clinicians maybe include PT, OT, social workers, psychologists, dietitians.
There are three groups that will not participate in MIPS. Those who are in their first year of Medicare Part B participation will not be required to participate in MIPS. Also, those who are below the low patient volume threshold, which would include those who have Medicare billing charges less than or equal to $10,000 and provide care for 100 or fewer Medicare patients in one year. The third group is those who are participate in advanced alternative payment models.
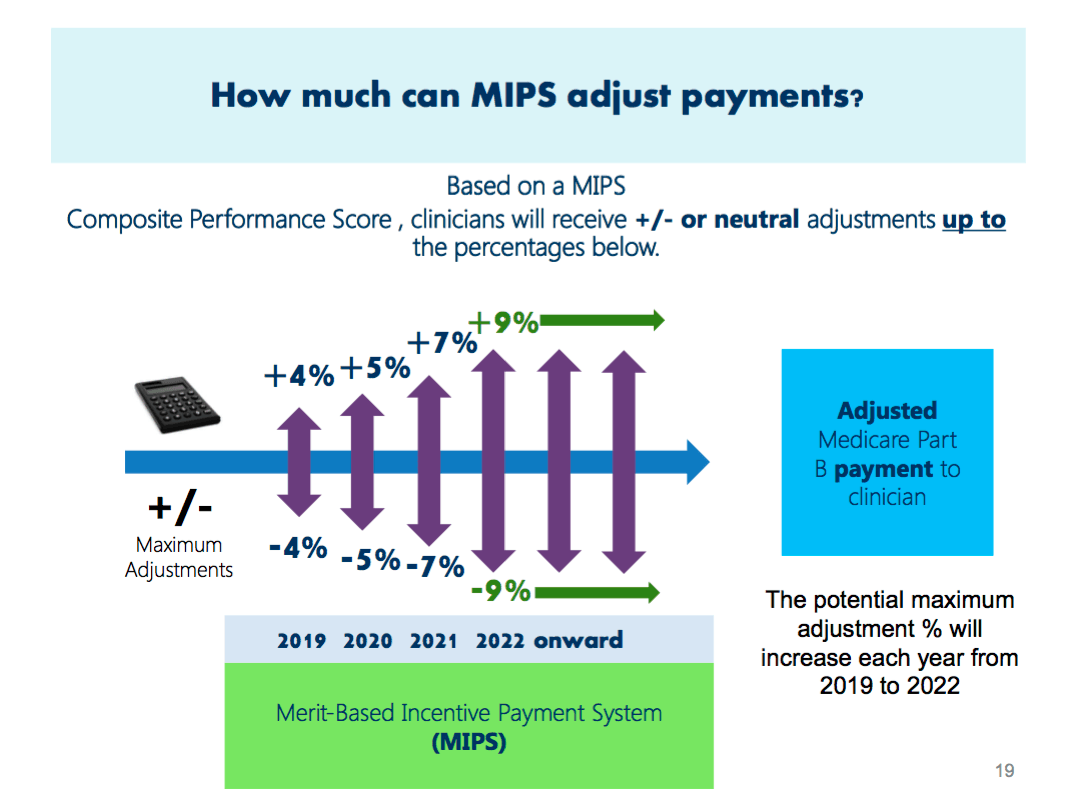
MIPS and Payments
By participating in MIPS you earn a payment adjustment based on your score. MIPS is a budget-neutral program; for every person that gets a positive adjustment there is someone who will get a negative adjustment.
It’s a little like this – Jimmy, Johnny and Jack are all sitting down for dinner. There’s a large bowl of bread in the middle. Jimmy did all his chores and entered them into the computer and his garden has grown great so he gets to eat first. Johnny is next and gets his fill of bread. Then it comes to Jack and because he had a bad apple and didn’t have time to enter his chores in the computer he gets the leftover, but unfortunately for him Jimmy and Johnny already ate up all the bread so there is none left over for him so he has to go back to the kitchen and bake a new loaf, most of which will be eaten by Jimmy and Johnny.
Everyone that provides services to Medicare patients will get paid out of the same “bowl”. If you have good scores you’re going to be given a percent adjustment for doing what they ask; and since everyone is eating out of the same bowl if someone gets a positive adjustment that means someone must be given a negative adjustment.
Participation in MIPS
If you’re not sure if you need to participate in MIPS you can check online using your NPI.
The data collection for MIPS started in 2017 with payment adjustments starting in 2019. If you’re a Medicare Part B clinician you should be taking part in MIPS. If you have not heard from your employer that they are collecting data you should ask how this is being addressed so you’re not behind.
You can report as an individual or as part of a group. “An individual is defined as a single clinician, identified by a single National Provider Identifier (NPI) number tied to a single Tax Identification Number (TIN)”; and “a group is defined as a single Taxpayer Identification Number (TIN) with 2 or more eligible clinicians (including at least one MIPS eligible clinician), as identified by their National Provider Identifiers (NPI), who have reassigned their Medicare billing rights to the TIN.”
I work for a multi-specialty private practice and due to the complexity of having different specialties with different measures the group decided to report as individuals. The problem is that if you report as a group everyone has to have the same measures, so what might be relevant to family practice is going to be different for orthopedics.
Also, from a payment perspective you risk having a negative adjustment for the whole group compared to each individual provider. For small private practices it might be easier to report as a group.
[jetpack_subscription_form title=”Don’t Miss Out on PA Billing Issues” subscribe_text=”Enter your email address to receive future posts by email for FREE” subscribe_button=”Sign Me Up”]
Where Does the MIPS Score Come From
There are four weighted performance categories that are going to contribute to the composite performance score. The four categories include quality, resource use, clinical practice improvement activities and advancing care information. Each category will have a different weight to it, so for the first year the quality category is going to be 50% of the total score.
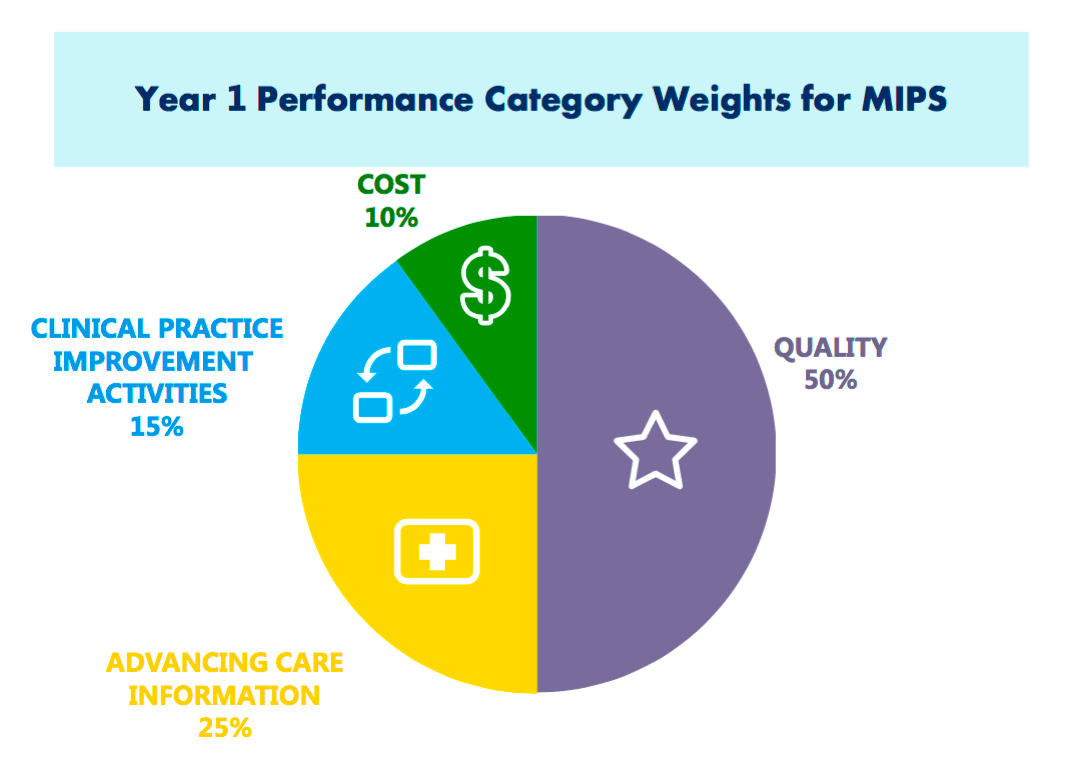
For the quality performance category you will be able to select six measures. The measure can be selected individually or can be a specialty measure set, and will have emphasis on the outcome of the measure. This is similar to the PQRS measures from before but it has been reduced from nine measures to six.
The resources used category will compare resources used across practices for similar care episodes and condition groups. This will be calculated based on claims so no reporting will be necessary for clinicians.
The clinical practice improvement activity focuses on ways to improve the practice. A minimum of one activity is required from a list of more than ninety proposed activities. Examples of improvement activity include care coordination, shared decision-making, safety checklist and expanding practice access. Full credit will be given for patient-centered medical homes.
The last category is advancing care information and this will be measured based on how you use electronic health records. The scoring for this category is based on measures of patient engagement and information exchange.
Why You Should Care
I have talked to other providers who don’t know a lot about MIPS except for the fact that we’ve been told to push certain buttons to help keep track of our progress and so they go about their business pushing (or not pushing) the right buttons; but another important piece is that your MIPS score is going to follow you. We often like to default to our billing department on billing issues but this may affect you as you look for other jobs.
If your current organization does a poor job of meeting the quality metrics and it affects your score and later on you decide to change jobs but have a low score, a future employer might not want to take you on as it is going to affect how much Medicare pays. I’m not saying that it is right or fare that providers are judged on their MIPS score but when it comes to employers they do like to look at their bottom line so if you have a low score and that is going to affect your payments is a new employer going to want to take that on?
On the opposite side of things if you’re looking for a job it might be important to work with an employer who has providers with good MIPS scores as they are most likely doing things “right” in the eyes of Medicare.
Currently this is a Medicare only plan. It has not reached private insurances but as things go, private insurance typically follows Medicare; so even though your MIPS score may not affect all your payments right now, in the future it might.
I’ve noticed that with government policies there is a lot of question until things actually happen. At this point there are still a lot of questions with MIPS and as time goes on things will get clearer. Also, with the current presidential administration things can change as well. It’s not always the most fun topic to stay up to date on but it is important to know what is going on and make sure your employer is doing their best to stay on top of things as well; and in the mean time keep pushing those buttons and get the mips out of here.
Don’t forget to comment below the original post, sign up to receive future posts by email and share with your friends!